The thinking behind strategy communication
The development of a strategy can be a case for change, a new service, or a further development of an existing service and can involve major changes or relatively minor changes. But with any change, certain elements need to be in place. Even
small changes can make a difference to the quality of care (Rowe 2008).
The development of strategies within health care can be devised at a local or national level, and encompass a different size of area, or focus upon a specific topic or aspect of health. The strategy can be formulated through individual or cross-departmental /agency or cross-government programme. The majority of government strategies are currently developed with following a period of consultation with a wide variety of partners.
When we are communicating strategy, we are communicating change. The key for communicating strategy is to be able to align the extent and scope of the change and the approaches of implementation with the values and principles outlined in the
related policy document (Jones 2008).
Hunter has observed that, “regardless of the precise nature of a policy or strategy, and the support that exists for it, if the means to implement it are either non-existent or inadequate in terms of capacity or capability, or both, then it will count for little” (Hunter 2007:20). However, some organisations communicate their strategy really well. They manage to communicate what they want to achieve and how they will go about it. They get people motivated and remove the blocks that have prevented the strategy from working in the past; blocks that may be embedded within the culture of the organisation. They get people behind the strategy, adding to it and making it work in their part of the business. In short, they make it happen (Jones 2008).
There are key elements and activities that are known to affect the resources required for managing successful change efforts:
- motivating change: creating readiness for change and overcoming resistance
- creating a vision: mission, valued outcomes and conditions, midpoint goals
- developing political support: assessing change agent power, identifying key stakeholders, influencing stakeholders
- managing the transition: activity planning, commitment planning management structures
- sustaining momentum: providing resources, building support system for change agents, developing new competencies and skills, reinforcing new behaviours (French & Bell 1999).
These elements are very similar to Kotter’s 8 Steps
The guidance to support strategy implementation
Executing a strategy is perceived as more difficult than its development and represents a disciplined process or a logical set of connected activities that enables an organisation to take a strategy and make it work (Hrebiniak 2005).
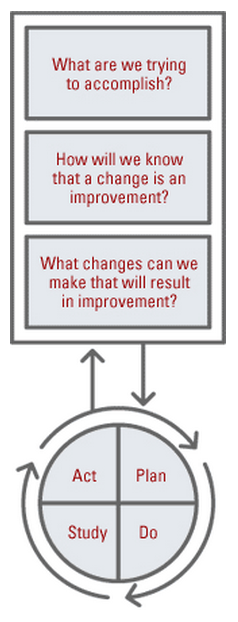
The process of quality improvement is of key importance to the health and social care system and the use of a continuous cycle of planning, implementing strategies, evaluating the effectiveness of these strategies and the use of reflection to see what further
improvements can be made.
The plan, do, study, act (PDSA) model for improvement, was designed to provide a framework to develop, test and implement changes which lead to an improved service. By ensuring that there is a clear understanding of what is to be achieved and how measurement of the change will occur ideas can be tested using PDSA cycles. One of the strengths of PDSA is the reversibility i.e. if the change does not work, normal working practice can be resumed, and another option trialled.
https://improvement.nhs.uk/documents/2142/plan-do-study-act.pdf
Also see: Oxford handbook of public health practice, Edition 3, P422
The cycle takes us through a series of stages which can support strategy, service and programme development. The PDSA is a cycle of improvement that involves asking three key questions:
- What are we trying to accomplish?
- How will we know that a change is an improvement?
- What changes can we make that will result in an improvement?
The technique can be used at any stage to support effective strategic development.
Stage 1: Strategic analysis and planning
Strategic analysis usually involves detailed research into the market, consumers and customers, competition, and other factors in the external environment that will influence and affect the strategy. Strategic planning involves choices about what the organisation wants to achieve and which strategy is best suited to achieve it. From a health care perspective the choice and or development of strategy at a locality level will be in response to policy directives. This stage can be linked to the PLAN phase of the PDSA cycle.
A key issue at this stage is who is currently involved and who needs to be involved to take this forward. Identification of the key stakeholders and an assessment of their interests will therefore be paramount to effective analysis and planning. The use of a SWOT (Strengths, Weaknesses, Opportunities, Threats) analysis with key stakeholders at this stage can help to provide a subjective assessment of data concerning the strategic issues that will help understanding, presentation, discussion and decision making (see 5d: Understandingthe Theory and Process of Strategy Development: Theories of Strategic Planning).
Local mechanisms for involvement within the planning stages can also be introduced through local partnerships where discussion and integration of strategic priorities can be shared amongst partners (see 5b: Understanding Organisations, their Structure and Function: Intersectoral works, collaborative working practices and partnerships).
The process of creating and sharing a vision requires systematic scrutiny to confirm whether planned action is well understood and matches shared goals. The use of a prioritisation and planning tool provides a checklist to clarify planning processes as well as determining when projects are in a pilot or roll-out phase (Swanton and Frost 2007).
Planning Checklist (Swanton and Frost 2007:119)
|
Subject / priority / proposal…… |
|||
|
Questions |
Evidence |
Outputs/outcomes |
|
|
|
Existing |
Needed |
|
|
Do something |
Does evidence exist that show the need for action? |
What further evidence is needed to confirm need? |
|
|
What/who is the target? |
Is there clear evidence of the rationale for targeting? |
What further evidence is needed to confirm targets? |
|
|
How/where to intervene? |
Is there a clear understanding of the methodology and cause and effect chain? |
What further evidence is needed to define the methodology? |
|
|
What specifically could be done? |
What is the full range of potential action? |
Are there gaps in understanding? |
|
|
What specifically should be done? |
What is practical to deliver? |
Is there a need for feasibility tests? |
|
Stage 2: Strategic design and implementation planning
The next stage is to detail the strategy, design how it will be implemented and plan that implementation. This stage can also be linked to the PLAN phase of the PDSA cycle.
There are a number of barriers to implementing change in a health setting. Barriers can be psychological, social, cultural, environmental and economic. Overcoming such barriers is clearly a key to success.
From an organisational perspective, the key is to consider which areas of the organisation’s behaviours are likely to hold back the implementation of the strategy and address them. At an individual level, a number of models that describe the stages that people go through when change occurs are just as important for implementing strategy as they are to behaviour change. Therefore when strategy is planned, designed and implemented it tends to go through a number of stages that can be aligned to the developmental, transitional and transformational types of change models. What is important is to understand the levels of change that all stakeholders will need to go through in order to implement the strategy effectively (see 5c: Management and Change: Critical Evaluation of a range of principles and frameworks for managing change).
From a community perspective, approaches for engagement with community stakeholders can be found within the approaches of social marketing which puts the consumer at the centre of all policy development and delivery work and concentrates resources around delivering key public health messages through the wider stakeholder community.
For example the aims of a social marketing approach to tackling obesity would be to:
- identify the drivers of families food and physical activity habits
- establish motivations and barriers preventing people from adopting healthier behaviours
- inform the programme’s communication and intervention strategies
- help contribute to the programme’s evidence base.
Using the techniques within social marketing’s would create:
- a behaviour change strategy to identify:
- broad support from stakeholders
- family based solutions required
- balance of physical activity and food habits
- audience segmentation
- identify high risk audiences
- information provision is sufficient
- partnership programme
- willingness for more coordinated working
- risk (organisational cultures) & benefits (delivering priorities)
- remaining issue over duplication (child focused & information driven)
(http://livegroup.co.uk/tacklingchildhoodobesity/SE/index.php).
(see 2i: Disease Prevention, Models of Behaviour Change, An Understanding of Social Marketing).
A futher way to overcome barriers is through the direct involvement of the public and patients (see 5d: Understanding the Theory and Process of Strategy Development: Stakeholder engagement in policy development, including its facilitation and consideration of obstacles / public and carer consultation and involvement in health service planning)
Stage 3: Launching the strategy
Before the launch of the strategy, plans for communication should be prepared that include what will be communicated, when, by whom and at which events. A key issue is the ability to manage communication about the strategy as part of the implementation process. Drucker’s (2007) discourse on management challenges within the 21st Century can be considered in relation to effectiveness in health care organisations and the need to understand the people who one works with and depends upon. This stage can be linked with the DO phase of the PDSA cycle.
The environment for communicating about health has changed significantly. These changes include dramatic increases in the number of communication channels and the number of health issues vying for public attention. There are a number of ways of communicating messages and some of these can also be used to communicate health messages. These can be divided into five categories:
|
Communication Category |
Example of Communication Medium |
|
Intrapersonal |
Internal communication (e.g. what we think, when we listen to an inner voice) |
|
Interpersonal |
One to one, small group, emails, telephone calls and other activities that allow personal listening and response |
|
Organisational |
Lectures, seminars, debates, meetings, memos, intranets, newsletter, workshops, displays |
|
Community |
Local radio, talks, seminars, debates, local newspapers, bill boards, bus tickets, health fairs |
|
Public/Media |
Newspapers, television, radio, internet, , mobile phones, social media |
Approaches within the field of ‘Health Communication’ encompass the study and use of communication strategies to inform and influence individual and community decisions that enhance health.
Stage 4: Follow-up and commitment
After the launch of the strategy initial results of the implementation processes should begin to come through, however it is important to plan to reinforce the messages with stakeholders and the wider community on a regular basis. The duration
between reviews however is known to make a significant difference to maintaining commitment and involvement (Jones 2008). This stage can be linked to STUDY phase of the PDSA cycle.
Irregular or periods of more than two month apart between reviews can weaken the credibility of the reporting process. Scheduling milestones, gaining commitment to them and tracking progress are the simple ways to ensure success. The amount of
effort that people are able to put into a change programme alongside their existing work is also a factor.
A range of information can be used within follow-up processes and the table below suggest some areas of data collection and measurement that can provide both qualitative and quantitative feedback. A wide variety of activities may be undertaken in
order to implement the strategy and the use of evaluation questions and evaluation methods based upon appropriate types of data analysis can support monitoring and evaluation strategies. The table below summarises the broad types of interventions
used in tackling obesity (see Interventions and Evaluation methods for tackling obesity http://www.dh.gov.uk).
|
Type of initiative |
Evaluation questions |
Evaluation methods |
|
Awareness-raising campaigns |
Which cluster groups(s) changed their attitudes towards healthy eating and in what ways? How many articles were published in the local media and what was the content? |
· Cross-sectional surveys · Focus groups · Content analysis of media |
|
Public participation |
How can more people become physically active? Should GPs be providing more advice? |
· Focus groups · Questionnaire surveys |
|
Interactive events (outreach, theatre, demonstrations) |
How many and what type of people attended the event? How engaged was the audience? In what ways did participants’ views of obesity change? |
· Exit polls · Quota sample · Analysis of attendance records · Observation · Interviews |
|
Education and training |
How many healthcare professional attended obesity training courses? How many overweight and obese patients were provided with advice by healthcare professionals? |
· Statistical analysis · Questionnaire surveys · Interviews |
|
Ongoing profile-raising |
To what degree and in what way is obesity covered in the popular media? What contribution does profile raising investment make to obesity policy and improving the knowledge base? |
· Content analysis of sample of newspapers · Citation analysis of academic journals |
|
Targeted access and inclusion actions |
Are minority ethnic groups more receptive to advice on healthy eating or physical activity than the general population? Has this had an effect on the number of obese people in the target cluster group? |
· Statistical analysis · Questionnaire surveys |
|
Policy actions |
Has the implementation of the consultation exercise created new partnerships? |
· Focus groups · Documentation · Analysis |
|
Horizontal and supporting actions |
How many schools are taking part in the National Child Measurement Programme? |
· Statistical surveys · Documentation · Analysis |
|
Operational reviews |
Which public engagement approach is most cost effective? |
· Process evaluation · Cost-effectiveness · Analysis |
Stage 5: Embedding the strategy and tracking results
Strategy design and implementation is a continuous process. Continued communication about key themes and the resulting behavioural changes should be identifiable and will need to be updated as evaluation strategies are embedded into the process.
This phase can be linked with the ACT phase of the PDSA cycle and leads to recommendations and changes within the strategy and subsequent programme. The two basic rules for successful evaluation:
- The evaluation process must be thought through from the start, at the same time as developing the strategy’s aims, objectives and targets.
- Adequate funding must be set aside for evaluation.
The key areas to evaluate must be agreed among the partners, including participants, to reflect different agendas. Evaluation will include:
- Measuring indicators of progress, including progress towards targets
- Assessing how well various aspects of the strategy were perceived to work from the point of view of professionals from all sectors and by communities,
- And assessing whether the changes were a result of the intervention (Swanton and Frost 2007).
The use of an impact screening tool can encourage a more realistic perception of the likely impacts of the strategic goals upon particular population groups, and can be used during all stages of planning and review, as highlighted below:
Impact screening Tool (Swanton and Frost 2007).
|
Subject / priority / proposal…… |
|||
|
Certainty of efficacy |
Potential impact on the population |
||
|
|
Low |
Moderate |
High |
|
High There is a high degree of success |
Successful interventions but for relatively small population |
Successful interventions but would require roll-out across large population group |
Successful interventions that by their nature affect the whole population |
|
Medium There is some evidence of success |
Some evidence of success but only for small population |
Some evidence of success but not effective for whole population |
Some evidence of success, with the potential to reach the whole population |
|
Low There is limited evidence of success and/or evidence is limited to unique circumstances |
Little evidence of success and for small population |
Little evidence of success and not effective for whole population |
Little evidence of success but has focus on whole population |
The following set of questions can help assess the overall success of the strategy and the need for review and amendment:
- Were the objectives of the strategy met?
- Did the original objectives remain in place?
- What has actually been implemented?
- Has the problem itself changed?
- What relevance does the strategy now have?
- What were the outcomes? Were they anticipated or not? (Guest 2008).
References
- Borkowski, N. (2005) Organizational Behaviour in Health Care USA: Jones and Bartlett Publishers Inc
- Corcoran, N 2007 Communicating Health, Strategies for Health Promotion London: Sage
- Davies, H T O.; Nutley, S M,; and Mannion, R (2000) Organisational culture and quality of health care Quality in Health Care Vol 9: 111-119
- Department of Health (2008a) High quality care for all: NHS Next Stage Review London: Crown
- Department of Health (2008b) Commissioning Assurance Handbook London: NHS World Class Commissioning
- Drucker, P.F. (2007) Management Challenges for the 21st Century London: Butterworth-Heinemann
- French, W. and Bell, C. (1999) Organization Development. New Jersey: Prentice Hall
- Guest, C., Ricciardi, W., Kawachi, I. and Lang, I. eds., 2013. Oxford handbook of public health practice. OUP Oxford.
- Hunter, D (2007) Managing for Health London: Routledge
- Hrebiniak LG 2005) Making Strategy Work New Jersey: Wharton School Publishing
- Jones (2008) Communicating Strategy Hampshire UK:Gower
- Pencheon, D.; Guest, C.; Melzer, D and Muir Gray J.A. (2008) Oxford Handbook of Public Health Practice Oxford University Press
- Rowe, J (2008) Planning Public Health Strategies in Cowley, S Community Public Health in Policy and Practice London: Bailliere Tindall pp162-192
- Swanton, K. and Frost, M (2007) Lightening the load: Tackling overweight and obesity London: National Heart Forum
© S Markwell 2009, C Beynon 2017
