The steps in outbreak investigation including the use of relevant epidemiological methods
Outbreak Investigation
This section covers:
- The steps in outbreak investigation including the use of relevant epidemiological methods
- The Outbreak Investigation Process
- Sources of outbreaks
- Types of Outbreak – key facts
The Outbreak Investigation Process
Outbreak Investigation Team
If an outbreak is suspected an Outbreak Control Team (OCT) should be convened to conduct the investigation with the following represented in the membership;
- Consultant in Communicable Disease Control (CCDC)/Consultant in Health Protection (CHP)
- Environmental Health Officer (EHO)
- Consultant Microbiologist or Virologist
- Secretarial/Administrative support
With consideration of:
- Regional epidemiologist
- Media/press officer
- Infection control nurse
- State veterinary service
- Food chemist/microbiologist/Food Standards Authority
- Toxicologist
- Director of Public Health
- Water company
1. Confirmation of Outbreak
- Is there an increase in the number of cases expected in the population/time/place?
- Confirm numbers; interview cases, review laboratory findings
- Is further investigation needed? The extent and urgency of the investigation should be considered.
2. Verify Diagnosis
- Obtain medical records and laboratory reports
- Repeat tests if necessary
- Further clinical testing if needed
3. Case Definition
|
Component of case definition |
(Example) Hepatitis A Outbreak
|
|
Person Type of illness (e.g. “a person with…”) |
‘A person with an acute illness |
|
Place Location of suspected exposure |
which occurred after staying at Hotel X |
|
Time Based on incubation (if known) |
between Sep-Nov 2015 |
|
Clinical symptoms/Lab results |
with jaundice or elevated liver function tests |
|
Define population at risk |
of all residents and diners during this period.’ |
4. Case Finding
- Interview known cases
- Locate others exposed to probable risk factor
- Review routine surveillance data, notifications and laboratory results
- Contact other CCDC’s/CHPs, EHO’s, health workers
5. Descriptive Epidemiology
Using data collected it can be arranged by person/place/time into descriptive epidemiology.
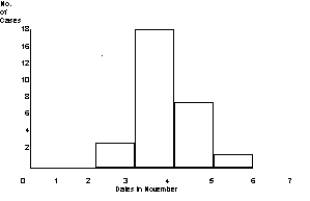
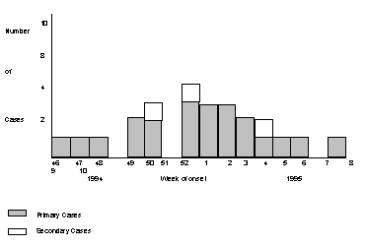
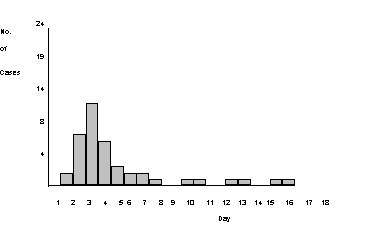
Epidemic Curve
Graph of occurrences of cases over time, this can help determine the nature of the outbreak:
- point (common) source
- propagated (continuing) source
- point source and person to person spread
Line List
A table summarising the information about persons associated with the outbreak.
Each row represents a single individual and each column represents a specific characteristic:
- identifying information
- demographics
- dates of illness/results
- pertinent risk factors
- exposures
- clinical details/lab results
6. Generate Hypothesis
Causes may have already been suspected, however, a formal hypothesis is helpful to establish after reflecting on the data interpreted in the descriptive epidemiology. It is useful for determining the most likely exposure that has caused the outbreak.
- Microbiological results of food/food/environmental samples (EHO to visit site)
- Veterinary investigation if appropriate.
7. Analytical Epidemiology
Useful to conduct analytical studies to test the hypothesis. If controls chosen appropriately this will reduce the bias in the studies performed.
- Assess exposures consistently between cases and controls (ill and non-ill).
Cohort Study
- Everyone potentially exposed
- Only use if a comprehensive list available
- RELATIVE RISK & ATTACK RATE= measure of association
e.g. Food based source outbreak at a wedding; guest list known,
Case Control Study
- Comparison of exposure amongst cases and controls.
- Useful study if complete list unavailable or is too large
- ODDS RATIO = measure of association, e.g. restaurant outbreak
8. Evaluate Control Measures
- Monitor incidence of cases once control measures enforced.
- Laboratory results useful for continued definitive identification of infectious agent in cases and if appropriate monitoring response to treatment/control measures.
9. Surveillance
- Documenting the effectiveness of control measures.
- Enhanced surveillance through laboratories and healthcare providers.
Control Measures
- Immediate control measures may be indicated from the start of the outbreak.
- Guided by epidemiological results and environmental investigation.
Control source
Animal/Human/Environmental
- Consider closing outlet
- Isolate and/or treat cases
- Destroy/treat food
- EHO to take samples if necessary
Protect persons at risk
- Consider prophylaxis (e.g. antibiotics)
- Improve hygiene / personal protective equipment if applicable
Interrupting transmission
- Depends on the mode of spread (e.g. bottled water if contaminated water supply with Cryptosporidium).
Communication
During outbreak
- Agree media strategy at initial OCT meeting and review at every meeting
- Information to the public and health professionals
After outbreak
- Outbreak report published and disseminated
- Recommendations made
Media Strategy
- Ensure accurate and timely information relayed
- Consider which type of media and for which groups; social media/secure comms/sensitive information/anonymity of cases.
- Media attention may be necessary if public action is required.
Sources of Outbreaks
Point source - explosive (primary cases will cluster within the range of the incubation period) e.g. Salmonella outbreak at wedding reception
Continuing source - e.g cases of S. agona PT15 by week of onset in England and Wales
Point source and person to person spread - e.g. E.Coli 0157 in a residential home
Types of Outbreak - key facts
Food/waterborne gastro-enteritis
- Involve Environmental Health Officer in investigation to find source.
- Collect stool specimens if possible from all sporadic cases; as many as possible in outbreak
Prevention
- hand washing and no towel sharing
- disposal of soiled material (use of plastic gloves/sealing; washing towels and linen on a 'hot' cycle)
- disinfect toilet area and taps daily
- education of personal hygiene and hygiene in preparation of food
Exclusions
- All cases must be excluded from work or school until free from diarrhoea and vomiting for 48 hours as a minimum
- In the case of an 'at risk' group, exclude for longer and consider the need for microbiological clearance before returning to work in:
- food handlers
- staff of health care facilities
- children under five years
- people with learning disabilities
In the case of 'non risk' groups there is no microbiology follow up
- most food poisoning - no screening of contacts necessary, except in the case of Typhoid and E.coli OI57
Exposures to infected water
Check:
- occupational exposure
- recreational exposure
- domestic exposure
- consumption of water, vegetables, fish (in areas of infected water)
(Source: Adapted from Public Health England. Communicable Disease Outbreak Management: Operational Guidance. Aug 2015)
Surveillance of international outbreaks
The WHO gathers reports of suspected outbreaks from a range of formal and informal sources. Formal reports are received from Ministries of health, WHO Regional and Country offices, national public health organisations, military and civilian laboratories, academic institutions, WHO collaborating centres and non-governmental organisations (NGO’s).
Informal sources such as social media, and electronic discussion groups provide epidemic intelligence also. The Global Public Health Intelligence Network (GPHIN) is a secure Internet-cased early warning tool that continuously searches international media sources to identify information about outbreaks of disease or public health events of international concern.
Everyday more than 20,000 online news reports (from over 30,000 sources) in nine languages are analysed[1]. More than 60% of initial outbreak reports come from unofficial informal sources, though verification is required. An alert is sent out if a potential risk is identified. This was instrumental in the SARS outbreak in China and was credited with the initial detection of MERS-CoV as well as an important role in the monitoring of the Ebola outbreak in West Africa.
(Source: Global Public Health Intelligence Network. WHO. Geneva. 2015)
© Sarah Anderson, Gayatri Manikkavasagan 2008, Kiran Attridge 2016
[1] Dion, M; AbdelMalik, P; Mawudeku, A. Big Data and the Global Public Health Intelligence Network (GPHIN). Canada Communicable Disease Report![]() 41.9
41.9![]() (Sep 3, 2015): 209-214.
(Sep 3, 2015): 209-214.
