Health Economics: 1 - Principles of Health Economics
From a Public Health point of view, health economics is just one of many disciplines that may be used to analyse issues of health and health care, specifically as one of the set of analytical methods labelled Health Services Research. But from an economics point of view, health economics is simply one of many topics to which economic principles and methods can be applied. So, in describing the principles of health economics, we are really setting out the principles of economics and how they might be interpreted in the context of health and health care. As Morris, Devlin Parkin and Spencer (2012) put it: Health economics is the application of economic theory, models and empirical techniques to the analysis of decision-making by individuals, health care providers and governments with respect to health and health care.
There are many different definitions of economics, but a definition given in a popular introductory textbook (Begg, Fischer and Dornbusch, 2005) is instructive: The study of how society decides what, how and for whom to produce. In analysing these issues, health economics attempts to apply the same analytical methods that would be applied to any good or service that the economy produces. However, it also always asks if the issues are different in health care.
1.1 Production, resources, scarcity and opportunity cost
The definition of economics above includes the term to produce, emphasising that economics deals with both health and health care as a good or service that is manufactured, or produced. All production requires the use of resources such as raw materials and labour, and we can regard production as a process by which these resources are transformed into goods:
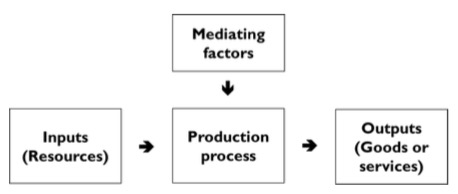
The inputs to this productive process are resources such as personnel (often referred to as labour), equipment and buildings (often referred to as capital), land and raw materials. The output of a process using health care inputs, such as health care professionals, therapeutic materials and clinics, could be an amount of health care of a given quality that is provided, for example. How inputs are converted into outputs may be affected by other mediating factors, for example the environment in which production takes place, such as whether the clinic is publicly or privately owned.
A key observation of economics is that resources are known to be limited in quantity at a point in time, but there are no known bounds on the quantity of outputs that is desired. This both acts as the fundamental driving force for economic activity and explains why health and health care can and should be considered like other goods. This issue, known as the problem of scarcity of resources means that choices must be made about what goods are produced, how they are to be produced and who will consume them. Another way to view this is that we cannot have all of the goods that we want, and in choosing the goods that we will have, we have to trade off one good for another.
The term economic goods is sometimes used to describe goods and services for which economic analysis is deemed to be relevant. These are defined as goods or services that are scarce relative to our wants for them. Health care is such an economic good: first, because the resources used to provide it are finite and we can only use more of these resources to create health care if we divert them from other uses; and secondly, because society’s wants for health care, that is what society would consume in the absence of constraints on its ability to pay for it, have no known bounds. Nowhere in the world is there a health care system that devotes enough resources to health care to meet all of its citizens’ wants.
Of course, in a national health system, it is likely that the aim is to meet needs rather than wants; this distinction is discussed below. But it is also the case that meeting one need may mean that another need is not met and that no-one has discovered a limit to need.
To summarise: in the economy as a whole, there are not enough scarce resources to meet all of the wants that people have, so we have to choose which wants are met and which are not met; in the health care system there are not enough health care resources to meet all of the health needs that people have, so we have to choose which needs are met and which are not met.
An assertion of economics is that scarcity, and the resulting necessity to choose between different uses for productive resources, applies everywhere in an economy and cannot be avoided. This is the premise underlying a key economics concept called opportunity cost. Producing any economic good or service means that the scarce resources that are used to create it cannot be used to produce other goods or services. If those other goods or services had been produced, they would have generated benefits to those who consumed them. The true cost of producing a good or service is therefore the benefits that are forgone by not producing other goods and services – in other words, it is the loss of the opportunity to create benefits by using resources in a different way. Because there are many possible goods and services that different combinations of resources could produce, the opportunity cost of using resources in a particular way is defined as the benefits that would have resulted from their best alternative use.
Costs in economics usually means opportunity costs. This concept is quite different to the more familiar idea of financial costs, which is the cost of goods, services and scarce resources in terms of the money that must be paid to obtain them. In practice, financial costs are very often used to measure opportunity costs, but this is not always the case. It is important to note that opportunity cost and financial costs are different ways of thinking about costs, not different elements of overall costs. They cannot be calculated separately and added together, for example.
1.2 Markets, Demand and Supply
1.2.1 Markets
Economics is a social science, as is emphasised in the definition of economics that refers to how society decides. Although society does make collective decisions about what, how and for whom to produce, in most modern economies this is largely done through markets, by the interaction of those who wish to buy (buyers, or consumers) and those who wish to sell (sellers, or suppliers).
Economics analyses markets mainly through what is called price theory. A market brings together the demand for goods from consumers and the supply of those goods from suppliers. Consumers and suppliers base their buying and selling on the price that they must pay or will receive. Price therefore acts as a signal to both groups as to what they should do in the market. Consumers will want to buy more if the price is lower, but suppliers will want to sell more if the price is higher. If prices are too high, then suppliers will not be able to sell all that they want to and may lower the price. If prices are too low, there will be consumers who cannot buy all that they want. As a result, consumers may bid more, or suppliers may see the possibility that they can raise their price but still be able to sell all that they want. Simple observable indicators like these, the presence of excess demand or supply, determine how much of a good or service is sold and the price that it is sold for.
This simple model of a market for a single good shows one way in which society decides for whom to produce. Consumers can obtain goods if they are both willing and able to pay for them; the more willing and the more able that they are, the more that they can potentially consume. Also, a strong willingness and ability to pay is reflected in high demand even at high prices, which signals to suppliers that they should supply more. So, scarce resources are allocated to producing goods for which demand is high rather than other goods for which the willingness and ability of consumers to pay is less. The demand for such goods is lower and their prices are lower. This, therefore, also shows how markets decide what to produce as well as for whom.
If we also assume that suppliers aim to make as much income as possible from what they sell, then they will wish to keep down the costs of production by choosing the most efficient production methods. So, markets also help to determine how goods are produced as well as what and for whom.
Of course, the real economy is far more complex than this and no economist would pretend that this simple model is a precise description of reality. But the point is that markets do not result in a random allocation of scarce resources, but one that is the result of the incentives provided to economic actors, both consumers and producers, by prices.
1.2.2 Demand for health care, demand for health and need
If we are considering the market for health care, we will be interested in the demand for health care. However, in considering this demand, it is important to recognise that health care has special characteristics that may make it different from other goods. One factor is that health care is not usually demanded because it is in itself pleasurable; in fact, it may be unpleasant. Instead, it is demanded mainly to improve health. So, even if health care is in itself unpleasant, it leads to more pleasure than would otherwise have been the case.
If health care is only demanded in order to improve health, is there then a demand for health improvements? Health can indeed be regarded as a good, in fact a fundamental commodity that is essential to people’s well-being, leading to a demand for improvements in it. Health does have characteristics that more conventional goods have; it can be manufactured; it is wanted and people are willing to pay for improvements in it; and it is scarce relative to people’s wants for it. However, its relationship with the demand for health care is not one-to-one, because although health is affected by health care, it is also affected by many other things and it also affects other aspects of welfare, not just health care. As a good, health is even more peculiar than health care, because of its characteristics. It is less tangible than most other goods, cannot be traded and cannot be passed from one person to another, although obviously some diseases can.
In the context of ordinary goods and services, economics distinguishes between a want, which is the desire to consume something, and effective demand, which is a want backed up by the willingness and ability to pay for it. It is effective demand that is the determinant of resource allocation in a market, rather than wants. But in the context of health care, the issue is more complicated than this, because many people believe that what matters in health care is neither wants nor demands, but needs. Health economists generally interpret a health care need as the capacity to benefit from it, thereby relating needs for health care to a need for health improvements. Not all wants are needs and vice versa. For example, a person may want nutrition supplements, even though these will not produce any health improvements for them; or they may not want a visit to the dentist even if it would improve their oral health.
The conclusion from this is that the demand for health care can be analysed as if it were any good or service, but it has peculiarities that may mean that the usual assumptions about the resource allocation effects of markets do not hold. Moreover, it may well be that people wish resource allocation to be based on the demand for health or the need for health care, neither of which can be provided in a conventional market.
The supply side of the market is analysed in economics in two separate but related ways. One is related to the resource input and goods output model outlined above, looking at how resource use, costs and outputs are related to each other within a firm. Some of the issues that this illuminates concern efficiency in production, which will be discussed below. Others include issues such as economies of scale - for example, are there any cost savings through having larger general practices?; productivity - for example, how many more surgical operations can a hospital provide if it hires an extra nurse?; and factor substitution - for example, does allowing dental hygienists to replace dentists in undertaking certain tasks lower the costs of producing dental care?
The other way in which supply is analysed is so called market structure - how many firms are there supplying to a market and how do they behave with respect to setting prices and output and making profits? There are two well-known theoretical extremes of market structure. Perfect competition has very many firms in the market so that none has any real economic power, none makes any profits, prices are as low as they can be and output is as high as can be. A monopoly has only one firm, which has great market power, makes as large profits as can be had and has higher prices and lower output. Other models are somewhere in between. The behaviour of some health care organisations, such as pharmaceutical companies, providers of services like dentistry, ophthalmic services and pharmaceutical dispensing and for-profit insurance companies can relatively easily be analysed using these models. It may be more difficult for other organisations. However, they may provide relevant insights, for example regulation of the UK provider sector is increasingly guided by the use of market forces involving contestability to provide some competitive pressures for efficiency.
1.3 Incremental analysis and the margin
Economics analyses many economic activities by according to marginal principles, which is a special case of what is called incremental analysis. Incremental analysis means that the effects of changes in the use of resources are examined according to how they differ from current use. Analysis is focussed on, for example, how much costs and benefits are increased or decreased due to a change in resource use, rather than the absolute levels of costs and benefits that exist after the change. The term ‘marginal’ means at the margin of an existing set of circumstances, for example the costs and benefits that will result from changing the allocation of resources to the smallest extent possible. It does not mean an unimportant change – the costs and benefits involved even in a small change in resource use could be very large. There are two reasons for analysing incremental and marginal changes. First, looking at incremental values of economic variables often gives a better view of the issues faced in decision making. Secondly, an influential economic theory suggests that people do, at least implicitly, make decisions using marginal principles.
A marginal change is defined as a change in an economic variable that is caused by the smallest possible change in another variable, often expressed as ‘one unit’ of that variable. For example, the marginal cost of a good or service is defined as the extra cost that is incurred by producing one more unit of it. That cost could be large, even though the change in the amount of the good or service is small. As an extreme example, suppose that the service is a particular surgical operation and the surgical unit performing it has reached full capacity for its operating theatre. Performing one extra operation would require a new theatre to be built, so its marginal cost would be very high.
However, the marginal cost of the last operation performed within the existing capacity may have been quite small, simply the cost of theatre staff, disposables and subsequent care. As this demonstrates, marginal cost may vary considerably with respect to the same size of change in the other variable, in this case one operation, depending on the absolute level of that other variable, in this case the number of operations already being performed.
A well-known example of the importance of looking at incremental costs is in assessing the impact of early discharge schemes that aim to lower hospital inpatient surgical costs by reducing length of stay. Hospitals may be able to calculate an average cost per day based on information on the average cost of an inpatient stay and length of stay. However, the costs of each inpatient day in practice differ over the time spent in hospital. At the beginning of an inpatient stay there are high costs of surgery and perhaps of high dependency care. At the end of the stay there may simply be basic nursing care and ‘hotel’ costs, which will be much smaller than the costs averaged over the whole length of stay. Reducing the number of low dependency days at the end of the stay will therefore save far fewer costs than might be expected by looking at the average. Incremental costs calculated with respect to an increase or decrease in the number of days would give a correct estimate of the likely savings.
Similarly, a marginal benefit is the extra benefit gained by the consumption of one more unit of a good – again, it is not a small or unimportant benefit. Consider a screening programme which can be carried out with different numbers of sequential tests. The more tests that are carried out, the more cases are detected. A programme that uses one test might yield 10 cases per 1,000 people tested, while a two-test programme might yield 11 cases. Looking at these in terms of their total yield, the two-test programme looks better than the one-test programme. But incremental principles focus on the marginal benefit, which in this case is 10 cases for the one-test programme and only 1 case for the two-test programme, which does not look so good.
Further use of the concept of the margin is discussed in section 6, and a specific application of this in health care is discussed in section 8.
1.4 Efficiency and equity
Economic analysis usually judges the way in which resources are used according to two main criteria: efficiency and equity. Efficiency refers to obtaining the greatest output for a given set of resources. Equity refers to a fair distribution of that output amongst the population. These two concepts have technical definitions, which are described below.
The technical definitions of efficiency described here use the labels given by Morris, Devlin, Parkin and Spencer (2012). Economists are specialists in the analysis of efficiency and largely agree about what it means, and about definitions of different types of efficiency. Unfortunately, however, the labels that they give to those types vary. The same concept may be given different names and the same name may be given to different concepts. So, if other texts are consulted, it may be wise to check what is meant if efficiency is referred to, especially if the terms technical or allocative efficiency are used.
A very broad definition of efficiency has been given by Knapp (1984): the allocation of scarce resources that maximises the achievement of aims. This is useful, because it suggests that the desire to achieve efficiency arises from the desire to improve the world. Given that resources are scarce and there are competing uses for them, we should aim to obtain the best set of uses, according to our definition of what ‘best’ means. If a country decides that the aim of its health system is to improve its population’s health and allocates a fixed budget to health care, it will obtain the biggest health gain if scarce health care resources within its health system are used efficiently.
Before examining more precise and technical definitions of efficiency, it is useful to understand an abstract economics idea called Pareto efficiency, which is sometimes also called allocative efficiency, though not consistently. This tries to define a criterion for judging different allocations of resources to different uses which might be widely acceptable. (Whether it is widely acceptable or not is debated, but that debate is beyond our aims here.) It asserts that we would be able to say that one state of the world is better than another if at least one person is better off under the first state compared with the alternative and no-one is worse off. This is called the Pareto criterion. If we change from one allocation of resources to another, for example changing the health care system in terms of the kind of care that is made available, and as a result some people get better care and no-one gets worse care, this is described as a Pareto improvement. If it is not possible to make any Pareto improvements, then we have achieved a Pareto optimum. A Pareto optimum is therefore a position where it is not possible to make anyone better off without making someone else worse off.
If the aim is to make people in general as well off as possible and there is no concern about whether some people are better off than others, then a Pareto optimum is efficient. Given a Pareto optimal allocation of resources, that aim cannot be achieved to a greater extent because even if one person, or even many people, could be made better off, we do not know if this is outweighed by the fact that some people, even if it is only one person, are made worse off. However, there is not one unique Pareto optimum; the existence of a Pareto optimum does not mean that this is the only efficient way in which resources could be allocated. There are many allocations of resources that would be Pareto optimal, some of which would imply great inequalities between different people. If our aims also took account of this, then we might not view all Pareto optimums as efficient.
Pareto efficiency is therefore a contentious idea as a way of thinking about how resources should be allocated at a societal level, but does form the basis of definitions of efficiency in economics more narrowly. We will examine three types:
- Technical efficiency
- Economic efficiency
- Social efficiency
The concept of technical efficiency is used in analysing the production of health and health care. Recall from section 1.1 that this is a relationship between resource inputs and outputs. Production is technically efficient if the most output possible is produced from a given set of inputs, or the fewest inputs possible are used to produce a given amount of output. For example, the number of patients that can be treated in an out-patient clinic depends on the number of medical and nursing staff that are available and other inputs. If the most that can be provided by one doctor and two nurses is 20 treatments each day, then it is technically inefficient to provide 19 treatments using that number of staff or to provide 20 treatments using more staff.
Another way to view this is that an efficient clinic cannot undertake more treatments without employing at least one more member of staff. It is therefore Pareto efficient: production is technically efficient for a given set of inputs if it is only possible to produce more by using more of at least one input.
The concept of economic efficiency has several alternative labels. One of these is cost-effectiveness, but that term should be used carefully, as will be explained in the section on economic evaluation. Technical efficiency is only concerned with how many inputs are used in production, while economic efficiency is related to the cost of those inputs. Economic efficiency is achieved if the most output possible is produced for a given cost, or a given amount of output is produced at the lowest possible cost. Using the example above, some aspects of the treatment provided in a clinic could be undertaken either by doctors or nurses. It might be equally technically efficient for 20 treatments to be provided each day by using one doctor and two nurses or two doctors and one nurse. But if we assume that doctors are more expensive to employ than nurses, then it will be economically efficient to use the extra nurse rather than the extra doctor. So, although it is necessary to have technical efficiency to be able to achieve economic efficiency, not all technically efficient ways of producing are economically efficient.
Another way to view this is that, given the costs of employing staff, an efficient clinic cannot undertake more treatments without them costing more to provide. As before, it is Pareto efficient: production is economically efficient for a given set of input prices if it is only possible to produce more by incurring greater costs.
Social efficiency is a much broader concept. Both technical efficiency and economic efficiency concern production, and if the supply side of the market achieves economic efficiency in every market, there is allocative efficiency in production for the economy as a whole. An equivalent concept for the demand side of the market is allocative efficiency in consumption where, given prices of goods, consumers maximise their utility. Social efficiency is where both of these are achieved. It means allocative efficiency in the economy as a whole, which is the same as the overall Pareto efficiency described earlier.
Social efficiency is not a concept that has practical use in health economics, but it is an important idea for debates about whether markets should be used in health care. It can be shown that if markets work perfectly, then they will produce a socially efficient economy. To some, this gives a presumption in favour of market provision. However, if markets do not work perfectly they will not produce a socially efficient economy. The questions are then how imperfect markets are and whether there are alternatives, such as government provision, that are better. It is also important as a basis for a form of economic appraisal called cost-benefit analysis, which is discussed in section 5.
1.4.2 Equity
Equity is always an important criterion for allocation of resources. However, it is observable that people attach more importance to equity in health and health care than they do to many other goods and services. Equity is an important policy objective in almost every health care system in the world. Economists have created some very useful ways of measuring equity, but apart from that economic analysis of equity is less clear than the analysis of efficiency and there is lower consensus amongst economists about it.
It is important to distinguish equity from equality. Equity means fairness; in the health care context this means a fair distribution of health and health care between people and fairness in the burden of financing health care. Equality means an equal distribution, but it may not always be fair to be equal. For example, it might be thought to be unfair both healthy and sick people are given equal amounts of health care. However, equity is often defined with respect to equality and inequality. For example, it may be considered equitable that people who have an equal need for health care should have equal access to it. This is a very common definition of equity. However, there could be others, for example:
- equal use of health services for equal needs for health care
- equal use of health services for equal willingness to pay for that use
- equal health outcomes for equal merit
- equal health care payments by people for equal ability to pay for that health care
- equal expenditure on people for equal health deficit
There is a useful distinction when using equity definitions like this, which also has roots in philosophy, between horizontal and vertical equity. Horizontal equity means the equal treatment of equals; for example, do people who have the same health needs have equal access to health care? Vertical equity means the unequal treatment of unequals; for example, do people who have worse levels of health have greater access to health care?
There are some equity principles that do not take this form. For example, the utilitarian principle is that the most desirable states of the world are those that maximise society’s welfare, even if that involves inequalities. The maximin principle is if there are inequalities in the distribution of resources, these must benefit the least well off. The free market principle is that any distribution of resources, even if it produces very large inequalities, is fair if it results from fair trading, with a fair starting point for trade. The principle of procedural justice might mean that the process used to decide on the allocation of health care resources between people should be fair.
It is likely that these equity principles will conflict with each other. But economics does not really have anything to say about which of these, or others, is the fairest. That is a normative question, based on individual or collective value judgements and may be best analysed using philosophical, legal and political analysis. Economics may be able to describe inequalities, but normative analyses is needed to make judgements of these are inequitable; for example, whether inequalities in health care use across income groups are inequitable.
A key element of defining equity is specifying what it is that is to be fairly distributed between people, sometimes called the ‘distribuendum’. In the examples above, possible candidates were given as ‘use of health services’, ‘health outcomes’, ‘health care payments’ and ‘expenditure’. More generally, three areas are commonly considered as the possible objects of equitable distribution: health; health care; and the finance of health care.
Equity in the distribution of health is almost always expressed in terms of inequalities in health between different socioeconomic and demographic groups within populations. Such health inequalities, particularly those that demonstrate that health status levels vary systematically and inversely with socioeconomic status, are always important in health policy debates within most countries and are a major concern of governments, depending on their political preferences. Many countries include reduction of inequalities in health as a key aim of their health policy. It may be argued that reduction in health inequalities is in fact the only real equity issue for public policy, because a concern for a fair distribution of health care derives solely from a concern about fairness in the levels of health that different members of society have.
Although inequalities in health are important to health economists, and derive to some extent from economic factors, the specifically economic contribution to the analysis of health inequalities is relatively small compared with that from many other disciplines (McIntyre and Mooney, 2007). The main contribution of economics is to analyse inequalities in health with respect to individual people rather than social groupings of various kinds, which has led to valuable contributions in the measurement of health inequalities (O'Donnell et al, 2007).
Horizontal equity in the distribution of health care mainly examines the extent to which people with the same need for health care make the same use of health care services. One problem with this is that it is difficult to assess in practice what equal need means and how it might be measured. For example, different socioeconomic and ethnic groups might have different use of health services because they have different levels of ill-health. Ill-health should affect such use and is a need factor. But socioeconomic status and ethnicity are not in themselves need factors and should not directly affect the use of health services. If we control for need factors and find that the use of health care services is affected by non-need factors, there is evidence of horizontal inequity, because people with the same need consume different amounts of care.
Vertical equity in the distribution of health care is usually interpreted to mean the extent to which people who have different levels of ill-health have different levels of use that are appropriate to that difference. This is even more difficult to measure and even to offer a precise definition of what it should be in practice
Vertical equity is the main focus in considering the finance of health care, in particular whether or not health care is financed according to people’s ability to pay. Essentially, this means the extent to which people who have different incomes make appropriately different payments for their health care. This is encapsulated in the progressivity of the health care financing system. It is to be expected that rich people will pay more for health care than poor people; this does not mean that the finance system has any bias towards rich or poor. However, in a progressive financing system, the proportion of a person’s income that is used to pay for health care rises as income rises. Regressive systems can and do exist, where even though rich people spend more money on health care than poor people, the proportion of their income that the rich spend is lower.
Horizontal equity in financing considers the extent to which people who have the same income, and therefore the same ability to pay for health care, make the same payments. Inequities could arise because of the financing system itself. For example health care that is financed by local taxation may vary across regions; or payments may be related to use of services but the incidence of ill health – and therefore use of services – varies across people who have the same income.
1.5 Discounting
See Section 5.
1.6 Time horizons
See Section 5.
© David Parkin 2017
