Equality, Equity and Policy: Balancing Equity and Efficiency
Efficiency
Efficiency refers to the allocation of limited economic resources to meet the healthcare needs of a society. There are several types of efficiency (more thoroughly described in module 4d Health Economics section 1: The Principles of Health Economics). Briefly:
Equity
Equity is the ‘fair’ distribution of benefits across the population. Section 1: The Concepts of Need and Social Justice outlines different approaches to the ‘fair’ distribution of resources, based on moral principles and theories of social justice.
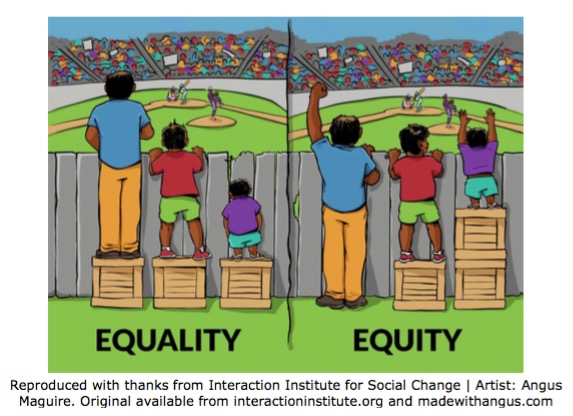
It is important to note that ‘equity’ differs from ‘equality’. Equality is the equal distribution of benefits across the population, so that every individual is given the same treatment regardless of their situation and ability to benefit from that treatment. Equal distribution of benefits does not always result in equal gains, as illustrated below.
The Utilitarian theory of social justice states that equity = equality. This is called end state equity – a situation where there is an equal distribution of benefits.
The Egalitarian theory of social justice states that equity is achieved when people have the same opportunities to obtain benefits even if the outcomes are unequal. This is called process equity.
Equity may apply to public health in several ways. For example:
- Equal health outcomes.
- Equal access to care for patients with equal need.
- Equal use of health care for equal need.
- Equal expenditure/resources of care for equal need.
- Equal costs (to the payer) for equal need.
There are two principles of equity in providing health care:
Horizontal equity: The equal treatment of individuals or groups who share similar circumstances.
Vertical equity: Individuals with different (or unequal) health should be treated differently (or unequally) in proportion to morally relevant factors. Morally relevant factors include ‘need’ (although see section 1: Need and Social Justice for the difficulties in establishing a definition of need), ability to benefit, autonomy. Morally irrelevant factors include gender, socio-economic status, income, education, ethnicity, disability, location, nationality.
It is debatable whether age should be considered morally relevant: according to the ‘fair innings’ principle of equity there exists a ‘normal’ healthy life span and individuals who have already achieved this are less of a priority than those who have not. (Williams, 1997 and Rivlin, 2000).
Achieving horizontal or vertical equity may involve re-organisation of services and redistribution of resources.
Balancing equity and efficiency
When prioritising health care the aim is to achieve efficiency (maximising health benefits given limited resources) whilst not compromising equity (fair distribution of resources). Some market economists may argue that equity and efficiency are mutually exclusive, however this doesn’t necessarily apply to health systems; indeed the 2000 World Health Report identified both equity and efficiency as important measures of a good health system.(Reidpath D et al, 2012)
There is no consensus on how to develop health policy that delivers maximum health gains whilst distributing resources fairly. Sassi et al. have outlined instances in which services could improve equity and/or efficiency outcomes, for example:
In the UK general practitioners receive a payment for every woman screened for cervical cancer. In spite of this incentive to universally offer cervical screening, some population groups (particularly disadvantaged groups) continue to have very low participation rates. Sassi et al. argue that more cases of cervical cancers would be avoided if targeted payments were introduced to general practitioners in order to increase screening rates equally in all socio-economic groups. Here, a focus on equal access instead of equal outcomes has compromised efficiency (Sassi et al, 2001).
When choosing between health interventions, James and colleagues (2005) propose scoring each health intervention according to explicit equity and efficiency criteria. They use cost-effectiveness as an efficiency criteria and the reduction of severe health conditions and poverty as equity criteria (in developing countries). Different weightings can then be given to each criterion so that policy makers can fully recognise efficiency and equity tradeoffs.
References
- Williams A (1997). “Intergenerational equity: an exploration of the 'fair innings' argument.” Health Econ. 6(2):117-32
- Rivlin MM (2000). “Why the fair innings argument is not persuasive”. BMC Medical Ethics 1:1
- Reidpath DD, Olafsdottir AE, Pokhrel S, Allotey P.(2012) “The fallacy of the equity-efficiency trade off: rethinking the efficient health system”. BMC Public Health; 12(Suppl1): S3.
- Sassi F, Le Grand J, Archard L (2001). “Equity versus efficiency: a dilemma for the NHS”. BMJ, 323: 762-763
- James C, Carrin G, Savedoff W, Hanvoravongchai P (2005). “Clarifying efficiency-equity tradeoffs through explicit criteria, with a focus on developing countries” Health Care Analysis, 13(1).
© Rebecca Steinbach 2009, Rachel Kwiatkowska 2016