Equality, Equity and Policy: Consumerism and Community Participation
Consumerism
In health services, consumerism is a social movement that seeks to promote and represent users’ interests (Black and Gruen, 2005). It suggests that users of health services should - and do - play an active role in making informed choices about health (Gabe et al, 2005).
The term ‘consumer’ originated in private business and indicates that in order to maximise profits, providers should consider the preferences of the buyer. In the absence of consumerism, providers may disregard consumer interests and therefore users’ rights need to be protected. The power of providers needs to be balanced by consumers who actively monitor and evaluate health services. Consumers have a choice of health care services and by exercising their right to choose, consumers can affect service provision.
Initiatives to strengthen consumer power involve (Saltman and Figueras, 1997, in Black and Gruen, 2005):
- better user information
- complaint-handling systems
- representation of consumers at various levels of health services
- mechanisms which protect patients’ rights
There are two broad approaches to protecting consumer rights in health care: (1) charters setting out entitlements and expectations and (2) laws. The UK has adopted the first approach and health care providers have developed explicit standards that patients can expect to receive, laid out in ‘The Patient’s Charter’ written in 1991 by the Department of Health, since superseded by the NHS Constitution. Other countries, such as the Netherlands, have legally defined patient rights (Black and Gruen, 2005).
Box 1: Consumerism in the NHS
|
The concept of ‘consumerism’ was first applied to users of UK health care in the late 1970s and early 1980s. The Conservative government of the 1980s and 1990s introduced a range of policies influenced by consumerist principles. For example, the government introduced general managers in the NHS in 1983 at different service levels to research patient needs and views about quality of care. The conservative government also introduced changes to the financial structure of the NHS (1990 NHS and Community Care Act) which aimed to increase competition and shift the culture of the NHS from “one determined by the preferences and decisions of professionals to one shaped by the views and wishes of users” (Gabe el al, 2005). The Patients Charter, written in 1991, set out rights and service standards that patients could expect and was designed to improve quality and make the NHS more responsive to individual patients. The Labour government who came to power in 1997 embraced the notion of the public as consumers of healthcare. The ‘NHS Plan’ introduced in 2000 promised to enhance standards of care and increase patient choice through initiatives such as NHS Direct (a telephone helpline providing healthcare advice) and walk-in centres (consultations available with no appointment needed, available in evenings and at weekends as well as daytime). http://www.nhs.uk/NHSEngland/thenhs/nhshistory/Pages/NHShistory2000s.aspx The ‘NHS Improvement Plan’ published in 2010 under a coalition government placed further emphasis on patient choice, forecasting an increase in independent providers of healthcare alongside the traditional NHS services. The rationale for this ‘marketisation’ of health services in the UK was that it would encourage competition and innovation, driving up healthcare standards and resulting in a system with the patient (consumer) experience at its core. Healthcare reforms following the publication of the Health and Social Care Bill in 2011 have however attracted widespread criticism, as many believe the NHS is on a path to privatisation which will result in less efficient and poorer quality health care. (Leys and Player, 2011) |
Community Participation
Community participation involves a power-sharing relationship between communities and decision-makers.
There are varying degrees of power available to the community. Arnstein (1971) describes a ladder of degrees of citizen participation, providing a framework to aid consideration of how to involve the public.
Box 2: Eight rungs on the ladder of citizen participation
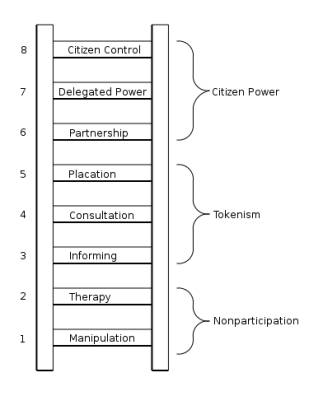 |
“The bottom rungs of the ladder are (1) Manipulation and (2) Therapy. These two rungs describe levels of "non-participation" that have been contrived by some to substitute for genuine participation. Their real objective is not to enable people to participate in planning or conducting programs, but to enable powerholders to "educate" or "cure" the participants. Rungs 3 and 4 progress to levels of "tokenism" that allow the have-nots to hear and to have a voice: (3) Informing and (4) Consultation. When they are proffered by powerholders as the total extent of participation, citizens may indeed hear and be heard. But under these conditions they lack the power to insure that their views will be heeded by the powerful. |
When participation is restricted to these levels, there is no follow-through, no "muscle," hence no assurance of changing the status quo. Rung (5) Placation is simply a higher level tokenism because the ground rules allow have-nots to advise, but retain for the powerholders the continued right to decide.
Further up the ladder are levels of citizen power with increasing degrees of decision-making clout. Citizens can enter into a (6) Partnership that enables them to negotiate and engage in trade-offs with traditional power holders. At the topmost rungs, (7) Delegated Power and (8) Citizen Control, have-not citizens obtain the majority of decision-making seats, or full managerial power.”
Source: Arnstein (1971)
The conceptual development of community participation in public health is primarily attributed to large multi-national health institutions, particularity the World Health Organisation (WHO). Community participation is one of the six principles underlying the primary health care approach to the Alma Ata declaration of The WHO Assembly in 1978. Its importance was re-affirmed in the Ottawa Charter of 1986. These international policies see community participation as a way for health systems to share some of the burden of prioritisation. It is a strategy that provides people with a sense of power over their own problems through careful reflection and collective action (Zakus and Lysack, 1998).
Communities can be involved in many aspects of health care. In Edinburgh and East Lothian there are a number of Community Health Initiatives: local charities, projects and groups who work with communities to improve health and reduce health inequalities. NHS Lothian and the city council support initiatives such as:
- Edinburgh Community Food, which has set up food co-operatives to give people access to fruit and vegetables in areas where they struggle to buy fresh produce.
- Edinburgh and Lothian Greenspace Trust, which works with local communities to develop green spaces and play areas to encourage outdoor activity.
Benefits of community participation for both the community and health services include (Zakus and Lysack, 1998):
For the community:
- A heightened sense of responsibility and conscientiousness regarding health.
- A more equitable relationship between providers and users.
- Decreased feelings of alienation.
- Greater diffusion of health knowledge.
For health services:
- The potential for greater access to fundraising opportunities (through community networks).
- Better understanding of community health needs, because services are more likely to be directed at ‘felt needs’ and carried out more appropriately.
Problems with community participation include (Zakus and Lysack, 1998):
- Conceptualisation: Communities are heterogeneous in terms of demographics, interests and concerns, leading to problems determining who is a legitimate representative of the community.
- Evaluation: The way in which community participation is expressed varies considerably in different contexts (see Box 2), making comparisons complex. As community participation is one of many concurrent strategies addressing particular health problems, measuring the effect of community participation on health outcomes is difficult.
- Representation: Ensuring adequate representation from different segments of the population (and the potential for those segments to have conflicting views).
The Health Education Authority (which has since been incorporated into NICE) commissioned a report on good practice in community participation in 1998 (Labyrinth Consultancy and Training, 1998). The results, stratified into 5 main topics, are presented in Box 3.
Box 3: Good practice guidelines for community participation in health projects
|
Clear and realistic role and remit:
Adequate and appropriate resources to meet the project remit:
Adequate and appropriate management and evaluation to support the project:
Recognition of the importance of the wider environment within which projects were operating:
Building in long-term sustainability:
Source: Labyrinth Consultancy and Training, 1998 |
For community development and empowerment see Module 2h: Principles and Practice of Health Promotion: Health Promotion Planning and Implementation in Settings and Communities.
References
- Arnstein S R (1971). “Eight rungs on the ladder of citizen participation”. in Cahn SE, Cahn E, Passett BA (eds) Citizen Participation: effecting community change. New York, Praeger Publications.
- Black N, Gruen R (2005). Understanding health services. Understanding Public Health Series. Open University Press: London School of Hygiene and Tropical Medicine.
- Gabe J, Bury M, Elston MA (2005). Key concepts in medical sociology. London: Sage Publications.
- Labyrinth Consultancy and Training (1998). A review of good practice in community participation health projects and initiatives: Summary bulletin. http://www.nice.org.uk/nicemedia
- Leys C, Player S (2011). The Plot. In: The Plot Against the NHS. Pontypool, Merlin Press.
- Saltman RB, Figueras J (eds) (1997). European health care reform: Analysis of current strategies. Copenhagen: World Health Organisation Regional Office for Europe.
- Zakus JD, Lysack C (1998). Revisiting community participation. Health Policy and Planning, 13(1): 1-12.
Weblinks
- NHS Health Constitution for England: https://www.gov.uk/government/publications/the-nhs-constitution-for-england/the-nhs-constitution-for-england
- Lothian Community Health Initiatives Forum: http://www.lchif.org.uk/about-us/
© Rebecca Steinbach 2009, Rachel Kwiatkowska 2016
