Principles and Practice of Health Promotion: Health Promotion Models and Theories
This section covers:
- The value of models in explaining and predicting health-related behaviour
- Theory and practice of communication with regard to health education
- Health education and other methods of influencing personal lifestyles which affect health
- Risk behaviour in health and the effect of interventions in influencing health-related behaviour in professionals, patients and the public (see also Health Promotion Evaluation and Effectiveness)
- The prevention paradox
- An understanding of social marketing
Introduction
This section describes a number of theories and models that have been used to explain and predict health behaviour, understand perception of risk and guide intervention and communication strategies. They also provide an insight into the development of health education and mass communication techniques, an understanding of their limitations, and recognition of the need for complex multifactorial interventions to promote health that recognise and address social, environmental and economic factors in the context of individual health behaviour. It covers: the Health Belief Model, Theories of Reasoned Action and Planned Behaviour, Stages of Change (Transtheoretical) Model, Social Cognitive Theory, Motivational Interviewing and brief interventions, Diffusion of Innovation Theory, the Communication-Behaviour Change Model, Social Marketing and communication as part of learning.
(A more detailed guide to theories and models can be found in: Nutbeam D & Harris E (2004) Theory in a nutshell: a practical guide to health promotion theories. Sydney, NSW, McGraw-Hill)
2.1 Models used to explain and predict health-related behaviour
Theories and models are used to organise knowledge in a systematic way that is applicable in a wide range of situations and circumstances, models help to provide simplified representations of the ways in which people think and act. In simple words, models provide practical means for applying theories. This allows the health promoter to hypothesise ways of intervening in order to change health-damaging behaviours. Most health promotion theories are drawn from other disciplines including psychology, sociology and management sciences. There is substantial evidence that the use of theory in designing and implementing health promotion programmes improves the effectiveness of interventions.
In order to simplify health-related behaviour and make it more readily understandable, models are usually generaliseable and emphasise simple relationships between individual behaviours and contextual influences. However, in real life the situation is much more complex. Models may attempt to operate at individual and societal levels, and the more they try to integrate individual, social, and cultural perspectives for example, the more complicated they become. Focussing on individual behaviour change is also only one aspect of health promotion. Well planned interventions will be multifactorial and operate across the different dimensions of the Ottawa Charter. For instance, as well as educating about and supporting behavioural change in individuals, they will include creating structural and systemic change in the availability of health-promoting local services, and influencing the public policy context through legislation and fiscal means. Effective health promotion operates in a number of dimensions at the same time to create the conditions for change, provide support to change, and to maintain healthy behaviours.
That said, a number of theories and models have been extremely influential in health promotion by informing the way we think about health behaviour and providing ways of conceptualising, predicting and changing health behaviour. Table 2.1 below summarises areas of health promotion action and the theories or models underpinning them (Nutbeam & Harris, 2004). This section will consider the first set of models that explain health behaviour change in individuals and communication theories. Relevant theories from the other areas of change are noted in other sections describing community development and partnership working. It is notable that some public health practice today still often draws upon an extremely simplistic and inaccurate 'model' of behaviour, one that suggests that changing knowledge (K), leads to a change in attitude (A) and thence to the desired change in behaviour (B). Many campaigns and educational programmes operate on this expectation, leading to inevitable frustration at their lack of uptake or impact. Each of the models below goes some way to explaining some of the reasons why behaviour change is much more complex than the KAB 'model' would suggest, and while none of them will predict all of the variance in individual behaviour they provide useful and well-tested pointers to the attributes that need to be considered in designing a health promotion intervention.
Table 2.1 Areas of health promotion action and related theories and models (Nutbeam & Harris, 2004)
| Area of change | Theories or models |
| Theories that explain health behaviour and health behaviour change by focussing on the individual |
Health Belief Model Theory of Reasoned Action / Planned Behaviour Transtheoretical (Stages of Change) Model Social Learning Theory |
| Theories that explain change in communities and community action for health |
Community mobilisation
Diffusion of Innovations |
| Theories that guide the use of communication strategies for change to promote health |
Communication for behaviour change Social marketing |
| Models that explain changes in organisation and the creation of health-supportive organisational practices |
Theories of organisational change Models of intersectoral action
|
| Models that explain the development and implementation of healthy public policy |
Ecological framework for policy development Determinants of policy making Indicators of health promotion policy |
Health Belief Model (HBM)
The HBM is one of the earliest models used initially to explain differential behaviour in utilisation of prevention programmes such as immunisation. Originating in the 1950's it was developed to explain how the likelihood of taking action on a particular health problem is dependant on four different types of beliefs or perceptions (Fig. 2.1). It predicts that protective or health promoting actions depend on the extent to which individuals:
-
Believe they are susceptible to the problem (susceptibility)
-
Believe that the problem has serious consequences (severity)
-
Perceive the benefits of the specified actions (benefits)
-
Believe that the benefits to action outweigh the perceived costs (barriers)
Despite the recognition that HBM is a psycho-social model and can only account for those aspects of behaviour that can be explained by attitudes and beliefs, it has provided a useful theoretical framework for over thirty years and has been applied to a wide range of health-related behaviours. However it has been shown to be most effective in relation to the behaviours for which it was developed ie uptake of screening and immunisation, rather than more complex and socially determined behaviours such as diet and smoking. As Nutbeam and Harris (2004) say, 'Changes in knowledge and beliefs will almost always form part of a comprehensive health promotion programme, and the health belief model provides an essential reference point in the development of messages'.
Figure 2.1 Health Belief Model
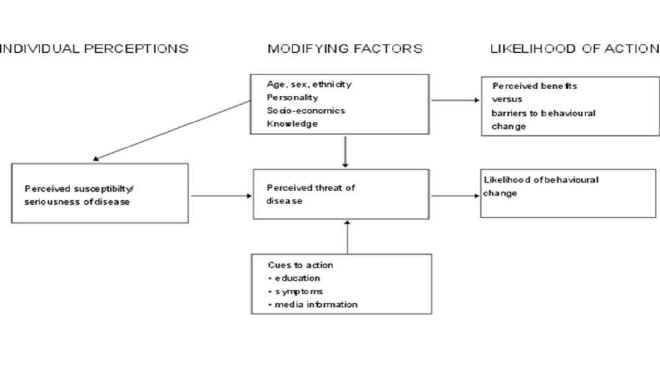
Source: Glanz et al, 2002, p. 52
Theories of Reasoned Action and Planned Behaviour
The Theory of Reasoned Action was developed by Azjen & Fishbein (1980) to explain behaviours under voluntary control, and assumes that people are rational and that the intention to act is the most immediate determinant of behaviour. Behavioural intentions are determined by attitudes, the belief that the desired beneficial outcome will occur if a particular behaviour is followed; and by subjective norms, that is the person's beliefs about what other people think they should do (normative beliefs). Later revisions of this model to the Theory of Planned Behaviour (Fig 2.2) included the incorporation of self-efficacy (Bandura, 1977). The model thus predicts that a person is more likely to change behaviour if they believe the behaviour will improve their health, is socially desirable and there is social pressure to change, and that they feel they have personal control over the behaviour and the ability to change. Self-efficacy is an important concept in social cognitive theory, it is concerned with self-judgements about how well one can execute courses of action, and can be very specific to individual behaviours. 'Self-efficacy judgements, whether accurate or faulty, influence choice of activities and environmental settings. People avoid activities they believe exceed their coping capabilities, but they undertake and perform assuredly those that they judge themselves to be capable of managing' (Bandura, 1982). This concept is indeed embodied in health promotion principles of empowerment and the Ottawa Charter definition of 'enabling people to take control of and improve their health'.
Figure 2.2 Theory of Planned Behaviour
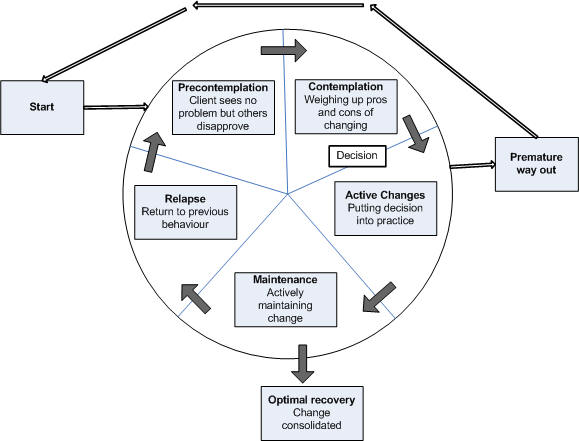
Stages of Change (Transtheoretical) model
This model was developed by Prochaska and DiClemente (1984) to explain the process of behaviour change. It describes different stages of motivation to change behaviour and indicates the need for different processes of change to support movement between stages. Behaviour change is not seen as a result of a single cognitive decision, but a series of steps.
-
Precontemplation: this describes individuals who are not even considering changing behaviour or are consciously intending not to change
-
Contemplation: the stage at which a person considers making a change to a specific behaviour
-
Determination, or preparation; the stage at which a person makes a serious commitment to change
-
Action: the stage at which behaviour change is initiated
-
Maintenance: sustaining the change, and achievement of predictable health gains
-
Relapse may also be the fifth stage
Based on study of addictive behaviours it also recognises that individuals may relapse and go back round the cycle again, and also that attention needs to be paid to the processes of maintaining behaviour change. The Stages of Change Model (Fig. 2.3) has been influential in design of smoking cessation programmes, and it has both an intuitive and practical appeal for practitioners in clinical settings. By understanding an individual's motivation, or readiness, to change (Rollnick et al, 1992) and applying behavioural techniques such as motivational interviewing that are appropriate to different stages, the practitioner can support an individual through a change process and understand why some people are more responsive than others to simple advice and support. For health practitioners the model helps them to see if the patient wants to make a change in a specified behaviour, the barriers that may need to be removed to make and sustain a change, and the fact that relapse is not a failure but simply a stage in a longer-term process of change.
A review of the application of the Transtheoretical Model to tobacco cessation and prevention showed that the validity of the model to tobacco use is strong and growing but not conclusive, and that interventions tailored to a smoker's stage were successful more often than non-tailored interventions in promoting forward stage movement (Spencer et al, 2002). The authors emphasise that practitioners should be aware of developments in the use of the model and that further refinement of processes of change and how they are operationalised in stage-matched interventions is needed.
Figure 2.3 The Stages of Change Model
Adapted from the work of Prochaska and diClemente
Social Cognitive Theory
Social Cognitive Theory (also known as Social Learning Theory) is valuable to health promotion practice in that it encompasses both the determinants of health and individual behaviours more comprehensively than other theories. It attempts to embrace the subtle and complex relationships between people and their environment, and the social and environmental influences on their actions. It builds on Bandura's work (1995) on self-efficacy and a greater awareness of the ways in which the environment shapes behaviour by making it more or less rewarding to behave in certain ways. For example, in the absence of legislation about smoking, if non-smokers are sufficiently assertive about not smoking it becomes more likely that a smoker will modify their behaviour. Thus the social influence has impacted on the individual's choice. This 'reciprocal determinism' describes the continuous interaction of the individual, their behaviour and the environment, and shows that the modification of social norms is a powerful health promotion tool. Further, personal cognitive factors play an important part, through the ability to learn a behaviour-reward pattern by observing others (observational learning), valuing the behaviours displayed by significant 'role models', and attributing positive 'expectancies' to the outcomes of for example avoiding smoking, or exercising more. Thus as well as social influence, peer influences and role models are also significant factors to consider in planning health promotion interventions.
The importance of self-efficacy in actually making behavioural changes is further recognised in this model, and both observational and participatory learning may be necessary to build up the knowledge and skills for developing the 'behavioural capabilities' for successful behaviour change.
References
Azjen & Fishbein (1980) Understanding attitudes and predicting social behaviour. Englewood Cliffs, NJ: Prentice-Hall
Bandura A (1977) Self-efficacy: toward a unifying theory of behavioural change. Psychological Review. 64(2): 191-225
Bandura A (1982) Self-efficacy mechanism in human agency. American Psychologist 37(2): 122-47
Bandura a (1995) Self-efficacy in changing societies. New York: Cambridge University Press
Nutbeam D & Harris E (2004) Theory in a nutshell: A practical guide to health promotion theories. Sydney, NSW: McGraw-Hill
Prochaska Jo and DiClemente CC (1984) The transtheoretical approach: crossing traditional boundaries of therapy. Homewood, Ill: Dow Jones Irwin
Rollnick S, Heather N & Bell A (1992) Negotiating behaviour change in medical settings: the development of brief motivational interviewing. J. of Mental Health 1: 25-37
Spencer L, Pagell F, Hallion ME & Adams TB (2002) Applying the Transtheoretical Model to tobacco cessation and prevention: a review of literature. American Journal of Health Promotion 17(1):7-71
2.2 Theory and practice of communication for health education
Skilful communication is an important part of the delivery of health information to both individuals and communities. As has been shown in the theories relating to individual health behaviour, the social influences operating within groups or communities of people are significant factors on their behaviour. While individual consultations with health practitioners and other interactions form an important part of health promotion, the individual's ability and desire to respond to health messages is mediated by their social group influences. Health promotion often employs influencing strategies at a community level, through mass media campaigns, education in schools or community groups. An understanding of the theoretical basis of communication to communities and to individuals is important for effective transmission of messages. However again, such strategies, while a fundamental part of health promotion, are best supported by other mechanisms such as structural and system supports.
Motivational interviewing and brief interventions
Motivational interviewing is an approach to behavioural counselling especially aimed at fostering the individual's desire to change. It was pioneered by an American psychologist in work on problem drinkers (Miller, 1983) and further developed for work with heroin addicts in the Netherlands and England (van Bilsen & van Emst, 1989). Using the Stages of Change model the technique recognises that at different stages people are in a different frame of mind about the behaviour concerned and have different motivations to change. Although many aspects of behavioural support (especially for smoking cessation) have been modelled around the principles of motivational interviewing, there is little evidence for the specific efficacy of 'motivational interviewing' as a technique, although there is evidence that a structured interviewing approach is more effective than an ad hoc one, (Dunn et al , 2001 and Maguire et al, 2001: cited in West et al, 2003). The key elements of motivational interviewing are presented below to indicate the types of skills that are helpful in supporting encouragement of motivation to change.
Van Bilsen described five important interactive criteria for successful interviewing:
-
Create a warm, comfortable and relaxing atmosphere
-
Give clear and concrete feedback to the patient about his behaviour, motives and personal situation
-
Structure and provide choice alternatives concerning the risk behaviour and its related problems
-
Stay in contact with the patient
-
Actively listen to the patient
Motivational interviewing is most appropriate for people at the contemplation stage when they are in conflict with their behaviour and are weighing the balance of 'to change or not to change'. Health or other professionals cannot force or manipulate change but can help patients in the process of making decisions that belong to them. Asking the individual to talk about their concerns and helping them to describe all the reasons why they should change puts more weight on the 'change' side of the balance. Motivational interviews may end with the individual feeling more motivated to think more about changing a behaviour, for others it may lead to making a decision to change, dependant on how ready they are. Motivational interviewing uses four key communication techniques as in Box 2.1.
|
Box 2.1 Motivational interviewing key communication techniques
|
A motivational interview consists of three phases; the 'eliciting phase', uses the key communication strategies and aims to get the individual to clearly state their concerns about a behaviour and lead them to the point where they see that change is necessary. The 'information phase' is when the patient is actively interested in their health and is seeking further information. In the 'negotiation phase' the focus is on what the patient wants to change, the means of achieving it and where to begin.
While structured behavioural support using these types of approaches is appropriate in specialised service by trained practitioners, there is now strong evidence that brief advice given by a GP in the course of a consultation, is effective in encouraging behaviour change such as in smoking cessation and increasing physical activity. Brief advice supported by written materials can produce a modest, short-term (6-12 weeks) increase in levels of physical activity (Hillsdon et al, 2005). For smoking, brief advice should consist of determining smoking status, giving advice to patients to stop and where agreed, making a referral to a specialist stop-smoking service where more behavioural support can be given. This approach is effective in encouraging 1-3% of smokers to give up for six months, which is over and above the natural rate of cessation in the population and independent of gender, age and presence of a smoking-related disease. The estimated cost per life year gained is £182, (West et al, 2004). The national standards for training in smoking cessation (HDA Expert Panel, 2003) incorporate principles of effective communication in their core content areas and key learning outcomes including, assessment of readiness to quit and commitment, addressing problems with motivation and providing behavioural support.
Diffusion of Innovation Theory
Diffusion of innovation theory derives from the systematic study of the ways in which new ideas are adopted by communities (Rogers, 1983, 2002). It describes five factors that determining the success and speed of innovation diffusion:
-
The characteristics of the potential adopters
-
The rate of adoption
-
The nature of the social system
-
The characteristics of the innovation
-
The characteristics of change agents
Adopters are categorised by the time it takes them to adopt the innovation. Rogers suggests the distribution in the population probably matches the normal probability distribution curve. Innovators are the 2-3% of the population quickest to adopt new ideas and early adopters as the 10-15% of the population who may be more mainstream within the community but are most amenable to change. In addition, there are those who may have the education, finances and social support available to them to readily adopt an innovation. The early majority are the 30-35% of the population who are also amenable to change and have become persuaded of the benefits of adopting the innovation. The late majority, (30-35%) are sceptics and are generally reluctant to adopt new ideas until the benefits have been established. The so-called laggards are the 10-20% who are most conservative and may be actively resistant to new ideas. However, of course it may also be that these are the least able to change due to poor financial, social and personal circumstances. This can be plotted as a classic S-shaped diffusion curve (Fig. 2.4)
So if we consider the example of passive smoking, many western countries have reached a stage where the majority of the public are in favour of a ban. The idea of the non-acceptability of smoking in public places has therefore reached the 'late majority' In the UK, the interest in and availability of organic foods has increased dramatically in recent years, probably moving from innovators who may have been thought to be unusual some years ago, to early adopters and now possibly the early majority.
Figure 2.4 S-shaped diffusion curve
Different innovations will take different times to disseminate through a population, and some may never penetrate fully. In health promotion terms attention needs to be paid to ways of maximising diffusion rates, and utilising appropriate strategies to engage and sustain different groups at different times. The characteristics of innovations that have been consistently associated with successful adoption include:
-
Compatibility with prevailing socio-economic and cultural values of the adopter
-
Clarity of the relative advantage of the innovation compared with current practices, including the perceived cost-effectiveness, as well as usefulness, convenience and prestige.
-
The simplicity and flexibility of the innovation i.e those that require simple actions and are easily adaptable to different circumstances
-
The reversibility and perceived risk of adoption, if perceived as high risk and requiring irreversible change they are likely to be less easily adopted
-
Observability of the results of adopting an innovation on others.
Another important factor for success is the professional worker or community member who acts as a 'change agent' and facilitates or supports the adoption of changes. Health promotion specialists may be considered as key change agents for health behaviours, although there will be many others who will also fulfil these roles. In terms of the community, community members can also act as role models to accelerate the adoption of change within their community.
The communication-behaviour change model
This model was devised by McGuire (1989) to guide public education campaigns. It is based on communication inputs and outputs designed to influence attitudes and behaviour, and can be helpful in conceptualising and designing mass communication strategies. Nutbeam (2006) considers this model demonstrates the difficulty of developing a public communication campaign that leads to sustainable behaviour change by itself. However although mass health communication campaigns have been based on this model in the past, today mass communication is more usually part of a comprehensive health promotion strategy, with more limited objectives of changing knowledge, attitudes and opinions rather than behaviour change itself. However it is still fundamentally important to get these messages right by paying attention to the five input criteria below.
-
Source - the person or organisation from whom the message is perceived to have come. The source can influence the credibility, clarity and relevance of the message.
-
Message - what is said and how it is said eg using fear or humour for different audiences
-
Channel - medium through which it is delivered eg TV, radio print, or more recently email and text messaging
-
Receiver - the intended target audience. Matching the right message to the right segment of the audience
-
Destination - desired outcome of the communication, change in attitudes, beliefs or behaviour.
Social marketing
The term social marketing was launched in the 1970's to describe 'the use of marketing principles and techniques to advance a social cause, idea or behaviour' (Kotler & Zaltman, 1971). Social marketing is considered different and similar to commercial marketing in the ways shown in Table 2.2:
Table 2.2
(adapted from Kotler et al, 2002)
| Commercial marketing | Social marketing |
| Selling goods or services | Selling behaviour change |
| Primary aim financial gain | Primary aim individual or societal gain |
| Market segments targeted that will provide greatest profitable volume of sales | Segments selected on basis of prevalence of social problem, ability to reach audience, readiness for change |
| Competition identified as other organisations offering similar goods or service | Competition the current or preferred behaviour of the target market |
| Customer orientation - the offer (4Ps - product, price, place and promotion) needs to appeal to target audience | |
| Exchange theory fundamental - benefits must equal or exceed costs | |
| Marketing research used throughout | |
| Audiences are segmented according to wants, needs, resources and current behaviours | |
| All 4Ps considered, not just relying on advertising | |
| Results are measured and used for improvement | |
A review of social marketing for health by the National Consumer Council states that it 'is not designed to replace other aspects of the public health. It is part of the toolkit that can be used in a strategic way, to inform the mix of interventions such as regulatory action, or practical hands-on methods to support specific behaviour change' (Mayo & French, 2006) They define health-related social marketing as 'the systematic application of marketing concepts and techniques, to achieve specific behavioural goals, to improve health and reduce health inequalities', and they cite benchmark criteria for effective social marketing summarised below in Table 2.3
Table 2.3 Social marketing benchmark criteria
| Benchmark | Explanation |
| Behavioural goals | Intervention seeks impact on individual or group behaviour. Behavioural goals are measurable and related indicators identified |
| Consumer research and pre-testing | Formative market research to identify audience characteristics and needs. Pre-testing and development integrated and range of sources used |
| Insight driven | Based on identifying and developing actionable insights rather than just data/intelligence. Focus on deep understanding of what motivates the consumer/citizen |
| Theory-based and informed | Theory drawn from different disciplines, and used to inform selection and development of appropriate intervention |
| Segmentation & targeting | More than simple demographic or epidemiological targeting, use of psycho-graphic data. Interventions tailored directly to audience segments |
| Marketing mix | Range of methods and approaches used to enhance impact |
| Exchange | Full analysis of costs/benefits to consumer. Attention to incentives and barriers, and maximising benefits of behaviour change |
| Competition | Consideration given to internal and external competition, including personal appeal of competing behaviours and external reinforcement. Consideration of impact of other interventions competing for attention of audience. |
The findings of the national review demonstrate the potential that social marketing approaches can have as part of a comprehensive mix of public health interventions in order to deliver public health goals. Understanding of the principles and practice of social marketing is considered to be underdeveloped across the wider public health system and when applied systematically social marketing can significantly improve impact and effectiveness of public health programmes.
Communication as part of learning
Communication is an integral part of learning, but while some approaches such as those described above consider that communication itself is capable of effecting change, others would refute this. As Tones and Green (2004, p209) state, 'whereas communication is a necessary pre-requisite for learning, it is learning per se that is responsible for change. The communication process is essentially concerned with the transmission and reception of messages and these may or may not result in learning.' While communication approaches may not in themselves be educational, any form of learning must include effective communication. Tones and Green (2004) describe three key components of the communication process:
-
A sender (communicator or source)
-
A message - this may take three forms, 'symbolic' meaning spoken or written language; 'iconic' referring to pictorial or diagrammatic representations, and 'enactive' describing situations where communication requires the active involvement of the audience
-
A receiver (audience)
They suggest that situations where there is active involvement of the audience, as in educational settings, are the most effective in potentially leading to both learning and change. Health education can be considered as persuasion, or as empowerment. Models that emphasise the characteristics of the sender and message in order to enhance communication, may be more of the persuasive or coercive form. However, empowerment as a central tenet of health promotion, would emphasise attention to strengthening the individual capacities of the receiver to question and challenge information sources and to create a more equal balance of power between communicators and receivers.
Risk communication
(for more information see: Rosenmoller et al (2006), Risk management, perception and communication, Chapter 11 in Davies M & Macdowall W (Eds) Health promotion theory: Understanding Public Health. Maidenhead, Open University, McGrawHill)
As has been shown in the discussions on models of health behaviour, decisions about whether to act on health advice are to a degree dependant on the individual's perception of risk. Risk perception depends on an understanding of the relationship of the behaviour with an undesirable outcome, and of the probability of that outcome occurring. Given both public and professional knowledge of probability is generally low this makes for difficulty in communicating risk in individual cases, although expert judgements are generally better than those of the public. Rosenmoller et al (2006) consider that the difference between actual and perceived risks is due to the cognitive inefficiencies in people's ability to judge small probabilities. Furthermore, other psychological factors that might be involved, include whether exposure to the risk is:
-
Voluntary vs. coerced (eg working in a nuclear plant vs. living in a nearby village)
-
Natural vs. industrial (eg sun radiation vs. telephone antennas)
-
Familiar vs. not familiar (car driving vs. canoeing)
-
Not dreaded vs. dreaded ( eg high blood pressure vs. cancer)
-
Chronic vs. catastrophic (car accidents vs. airplane accidents
-
Fair vs. unfair (riding a motorcycle at high speed vs. a pedestrian being hit by the same motorcycle)
The link between quantification of risk and the targeting of health promotion interventions has been described by Geoffrey Rose (1981) as the prevention paradox. Prevention Paradox arises because many interventions that aim to improve health have relatively small influence on the health of most people. Thus for one person to benefit, many people will have to change their behaviour and receive no benefit from these changes. It leads to the use of two distinct and complementary strategies, the 'high risk approach' and the 'population approach'. The pros and cons of these are summarised in Table 2.4 below.
Table 2.4 Advantages and disadvantages of the high-risk and population approaches
(adapted from French, 2006)
| Disadvantages | Advantages | |
|
High-risk approach Aims to identify those at highest risk and intervene to lower individual risk
|
Difficulties and costs of screening Not radical, does not address causes Limited potential for population health improvement Does not address social norms that frame health behaviour |
Intervention appropriate for individual Motivation high staff motivation also high Can be cost-effective Benefit-risk ratio higher for individual |
|
Population approach Aims to lower the mean level of risk in the population and shift the distribution of risk
|
Only a small benefit for the majority of individuals - (prevention paradox) Poor motivation to comply Possibly poor motivation of professionals due to less perceived effect Individual benefit-risk ratio may be a concern |
Seeks to remove root causes Large potential for whole population improvement Seeks to shift population norms |
References
- Dunn C, Deroo L & Rivara FP (2001) The use of brief interventions adopted from motivational interviewing across behavioural domains a systematic review. Addiction, 96 (12): 1725-42
- French J (2006) Targets, standards and indicators. Chapter 7 in Davies M & Macdowall W (Eds) Health promotion theory: Understanding Public Health. Maidenhead, Open University, McGrawHill
- HDA Expert Panel (2003) Standard for training in smoking cessation treatments. London, Health Development Agency
- Hillsdon M, Foster C, Cavill N, Crombie H & Naidoo B (2005) The effectiveness of public health interventions for increasing physical activity among adults: a review of reviews. 2nd Edn. London, Health Development Agency.
- Kotler P & Zaltman G (1971) Social marketing: an approach to planned change. Journal of Marketing. 35, 3-12
- Kotler P, Roberto N & Lee N (2002) Social marketing, improving the quality of life. California, Sage Publications
- Maguire TA, McElany JC & Drummond A (2001) A randomised controlled trial of a smoking cessation intervention based in community pharmacies. Addiction, 96 (2): 325-31
- Mayo E & French J (2006) It's our health! Realising the potential of effective social marketing. Independent review, findings and recommendations. London, National Consumer Council
- Miller W R (1983), Motivational interviewing with problem drinkers. Behavioural psychotherapy. 11: 147-52
- Nutbeam D (2006) Using theory to guide changing communities and organisations. In Davies M & MacDowell W (eds.) Health Promotion Theory. Understanding Public Health Series. OUP, McGrawHill,
- Rogers EM (1983) Diffusion of innovations. 3rd Edn. New York, Free Press.
- Rogers EM (2002) Diffusion of preventive interventions. Addictive Behaviours, 27: 989-93
- Rose G (1981) Strategy of prevention: lessons from cardiovascular disease. British Medical Journal 282: 1847-51
- Rosenmoller et al (2006), Risk management, perception and communication, Chapter 11 in Davies M & Macdowall W (Eds) Health promotion theory: Understanding Public Health. Maidenhead, Open University, McGrawHill
- Tones K & Green J (2004) Health promotion: planning and strategies. London, Sage Publications
- Van Bilsen H P & van Emst A J (1989) Motivating heroin users for change. In: G A Bennett (ed.) Treating drug abusers. Routledge, London
- West R, McNeill A & Raw M (2003) Meeting Department of Health smoking cessation targets. Recommendations for service providers. London, Health Development Agency
- West R, McNeill A & Raw M (2004) Smoking cessation guidelines for Scotland. Edinburgh, Health Scotland
© V Speller 2007
