PLEASE NOTE:
We are currently in the process of updating this chapter and we appreciate your patience whilst this is being completed.
Concepts of health, wellbeing and illness, and the aetiology of illness: Section 5. Stigma and how to tackle it
This section covers:
1. Causes and consequences of stigma
2. Ways to tackle stigma
1. Causes and consequences of stigma
Goffman (1963) defined stigma as ‘an attribute that is deeply discrediting within a particular interaction’. In other words, it is an undesirable characteristic in a particular context – for example, cohabitation before marriage was greatly frowned upon in England during the first part of the 19th century, but today is considered normal and is even encouraged. In some cultures it is still considered shameful to marry outside one’s faith or community, and many societies still do not permit the marriage of same sex couples. Stigma also occurs in a health context, with some diseases or conditions more stigmatised than others, e.g. mental illness and sexually transmitted infections tend to be stigmatised, whereas appendicitis or flu are not. Stigma may also vary within broader disease groups, such as cancer; lung cancer, for example, is more often stigmatised due to its strong association with smoking, and the perception that it is ‘self-inflicted’ (Chapple et al., 2004).
Stigmatisation is often a consequence of labelling, which can lead to an individual being treated differently or even excluded from society. For example, Jones (2012) discusses the stigmatisation of working class communities in England through the ‘chav’ label, arguing that it contributes to perpetuating social inequalities. Stigma may occur due to inequalities or marginalisation of certain groups (e.g. transgender people or sex workers), fear (e.g. not knowing how to deal with seizures or psychotic symptoms), or misinformation (e.g. the perception that HIV can be caught from toilet seats). These stigmas may be perpetuated by the media and certain groups or organisations (e.g. religious or political). Goffman's (1968) work is less concerned with the social process of labelling a particular action or pathological state as deviant, than with the stigmatising consequences of that process for an individual - what he referred to as 'The management of everyday life'.
All of us, including health professionals - because the medical model does not exist in a cultural vacuum - perceive certain conditions and disabilities as particularly stigmatising, as described above; an obvious example of this being HIV/AIDS. Thus, when a disease label is attached to a person, the very label itself has the power to 'spoil the sufferer's identity' (Goffman, 1968); both personal and social. The social stigma that results from this labelling process, derives not only from societal reaction which may produce actual discriminatory experiences ('enacted stigma'), but also the 'imagined' social reaction which can drastically change a person's self-identity ('felt stigma'):
'The stigmatised individual may be able to hide the discrediting attribute from others but cannot do so from him or herself'(Goffman:1967)
Felt stigma may manifest itself as feelings of shame, guilt or depression, and behaviours such as self-stigmatisation, withdrawal from society, and an unwillingness to speak up. Enacted stigma or discrimination may be direct, whereby a person is treated less favourably due to a defined characteristic, or indirect, where people from particular groups are more likely to suffer effects of rules, systems or procedures. Consequences may include the loss of employment, or denial of opportunities, abuse and violence, compulsory testing or quarantine, or denial of health services.
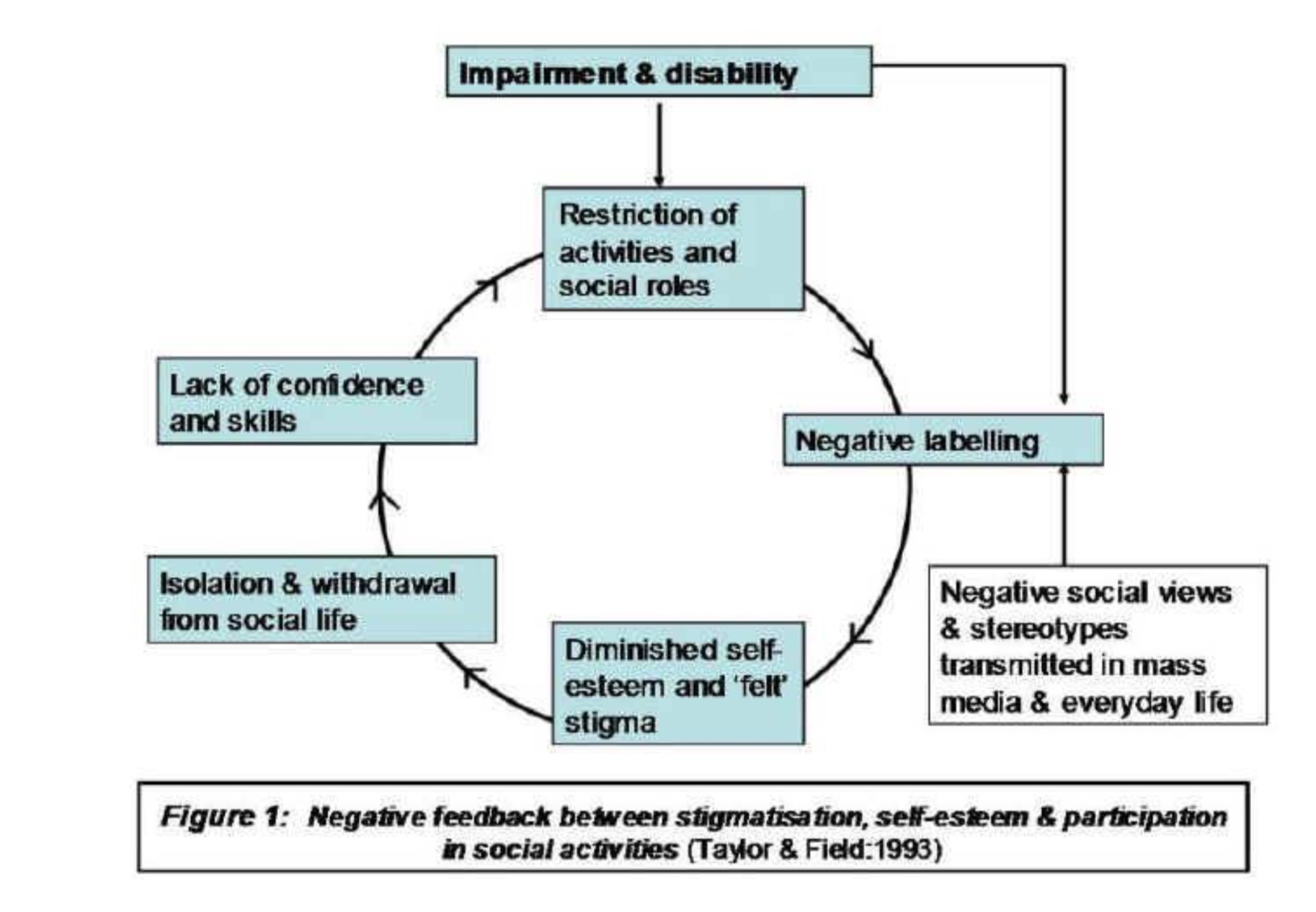
The impact of labelling and its consequences for stigmatisation can be represented as a negative feedback circle, which results in greater and greater diminution of social participation - this process is diagrammatically represented in Figure 1 below.
So for example, meeting the care needs of a child with a disability not only has a significant impact upon family members pre-existing work and social life patterns, but in addition families may also experience what is termed ‘courtesy stigma' (or 'stigma by association') because of their direct relationship to the child. The family may have to cope with their own feelings of shame or guilt, and may attempt to distance themselves in various ways from the disability.
In the case of diagnosing mental illness, the power to label is a significant one and is entrusted to the psychiatrist. Once an individual has been diagnosed as mentally ill, labelling theory would assert that the patient becomes stripped of their old identity and a new one is ascribed to them. This process usually leads to the labelled person internalising this new identity and social status, so taking on the role (‘master status') of the psychiatric patient with all its associated set of role expectations. Stigmatisation would then follow, which has the effect of excluding the labelled ‘psychiatric patient' from normal interactions. In this case, labelling theory focuses attention on the ethnocentric assumptions about ‘normal' behaviour held by psychiatrists which resulted in the misattribution of labels such as schizophrenia. This approach does not challenge the ‘fact' that high rates of psychopathology exist among black and Irish people, it simply claims that the wrong label is being applied with important consequences for these patients’ self-identity.
2. Ways to tackle stigma
Challenging stigma is beneficial to individuals and societies. For example, reducing the stigma of certain diseases or health conditions reduces barriers to seeking diagnosis and treatment; this benefits the individual through improving their health, and society by reducing the burden of disease in the population. In the case of communicable diseases such as chlamydia, diagnosis and treatment can also limit further transmission. On a social level, tackling stigma in marginalised groups helps to widen their participation in society and improves social cohesion.
In order to address stigma, there need to be changes in the attitudes and behaviours of both the stigmatised person and wider society. Positive challenges to stigma can change the attitudes leading to enacted stigma (discrimination), which in turn reduces felt stigma; this itself may reduce enacted stigma by changing behaviours such as self-stigmatisation and withdrawal, producing a ‘virtuous circle’. (see Lewis et al., 2014). Strategies to tackle stigma include the following:
- Legislation
It is possible to outlaw certain manifestations of enacted stigma, such as abusive behavior or denial of certain rights on the basis of a stigmatised characteristic. The UK’s Equality Act 2010 provides a legal framework for safeguarding the rights of people with the following protected characteristics: age, disability, gender reassignment, race, religion or belief, sex, sexual orientation, marriage and civil partnership and pregnancy and maternity. The advantages of implementing legislation are that it removes any ambiguity around what is acceptable, and can empower individuals to speak up. The main limitation is that although it may change behavior through introducing a consequence, it does not necessarily change attitudes. Someone who maintains a prejudiced or stigmatising attitude may comply with the legislation, but display subtle or unconscious stigmatising behavior. Nevertheless, if implemented effectively legislation can contribute to changing attitudes by denormalising inappropriate behaviour.
- Education
This may include public information campaigns to raise awareness of illness and challenge misconceptions and stereotypes. A current example is the Time to Change campaign launched in 2009 which aims to raise awareness about mental health and illness, including signposting to relevant support, and dispel common myths around mental illness. An evaluation published in the British Journal of Psychiatry (Evans-Lacko et al., 2013) concluded that the first 4 years of the programme had been effective in reducing stigma and discrimination by improving public attitudes and intended behaviour, though an improvement in public knowledge was not demonstrated. However, the overall positive impact of the campaign has been debated, with suggestions that it could actually increase stigma through the ‘othering’ of people with mental health problems.[1]
- Language
The Time to Change example highlights the importance of language in challenging stigma. Stigmatising language includes not only that which is derogatory or outwardly discriminatory, but also that related to labelling. For example, the term ‘schizophrenic’ implies that the individual’s identity is defined solely by their schizophrenia – so ‘person with schizophrenia’ is suggested as a more appropriate alternative. Another example is in the use of preferred pronouns to describe transgender people, including non-binary options.
- Public acknowledgement
Public acknowledgement may be that of the problem itself, or of potentially embarrassing or unpleasant symptoms. Public acknowledgement of problems is often done by those with social status such as celebrities; for example, the well-known actor and comedian Stephen Fry has endorsed the Time to Change campaign and spoken openly about his own experiences of mental illness,[2] which has been linked anecdotally to increases in numbers of people seeking help either for themselves or on behalf of family members. Celebrity deaths from a problem may also contribute to increasing awareness, and reduced stigma around help-seeking; following the early death from cervical cancer of reality TV celebrity Jade Goody in 2009, there was a significant increase in cervical screening attendance in England (Lancucki et al., 2012). Public information and awareness campaigns that openly discuss symptoms that people might find embarrassing can also help to reduce barriers to seeking diagnosis and treatment, such as Public Health England’s Blood in Pee campaign as part of the wider Be Clear on Cancer campaign.[3]
- Treatment
In a health and medical context, advances in the management of health conditions can contribute to reducing their visible signs that may contribute to stigma, whether physical characteristics (e.g. skin conditions) or behaviours (e.g. manifestations of mental illness). While it is generally accepted that efforts should be made to improve health and quality of life wherever possible, there is considerable controversy around intervening when the intended benefit is solely to reduce stigma – for example, the use of cosmetic surgery to ‘correct’ the facial features of children with Down syndrome, where the surgery carries physical risks with no medical benefits. It is argued that the onus should be on others in society to be more accepting, rather than on individuals with disabilities to change (Suzedelis, 2006). There is also debate around what constitutes ‘medical benefit’; for example, many people reject the medical view of deafness as an impairment or disability, instead claiming it as a culture and identity based on a trait (signified by the use of a capital ‘D’ for Deaf; see Jones, 2002). This is an important consideration in thinking about concepts of impairment, disability and handicap (see Section 6).
© I Crinson 2007, Lina Martino 2017
[1] 1:4 and stigma. http://www.bbc.co.uk/programmes/b04ntvvm/broadcasts
